A guide to the ACA for Maine businesses
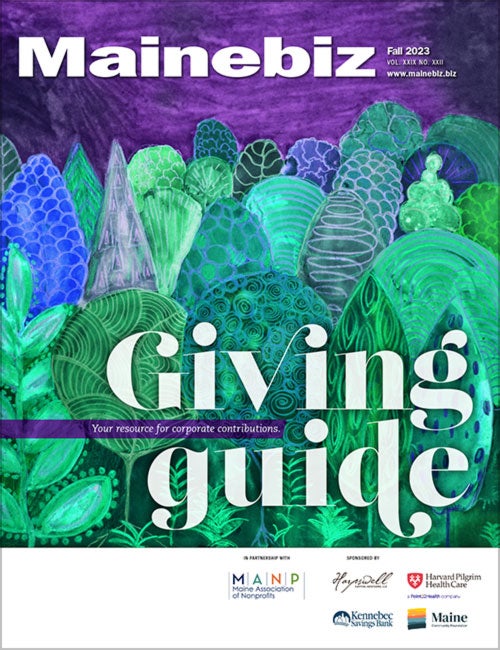
 PHOTo / Tim greenway
Ellen McPherson and Rick Morrone of Employee Benefits Solutions in Portland are gearing up to handle increasing questions about the rollout of the federal Affordable Care Act.
PHOTo / Tim greenway
Ellen McPherson and Rick Morrone of Employee Benefits Solutions in Portland are gearing up to handle increasing questions about the rollout of the federal Affordable Care Act.
Ellen McPherson, project and compliance manager for Employee Benefits Solutions, says the Affordable Care Act is no longer a “let's see if it's really going to happen” question for Maine employers. With President Obama's reelection and the return of a Democratic majority to the U.S. Senate, she says employers of all sizes are scrambling to understand what the law requires them to do, or not, in terms of providing health insurance for their workers.
Even for companies large enough to have their own human resources manager onsite, it can be a daunting task.
“It's in constant movement,” says Rick Morrone, director of Employee Benefits Solutions, the Portland-based company that provides administrative and brokerage services for group health, dental and other employer-offered insurance benefits. “We've identified this as something huge enough, with a significant impact on our industry and our clients, that we have full-time people like Ellen dedicated to staying on top of [ACA-related issues].”
McPherson and Morrone started doing ACA briefings for business groups across the state last summer. Signed into law by President Obama in 2010, the ACA has been slowly rolled out with grants supporting prevention and public health initiatives, a new coverage option for parents with children under age 26 who don't have job-based health insurance, and a slew of phased-in requirements for businesses large and small. The law's key provisions — the employer mandate for companies with 50 or more full-time workers and the launch of health insurance exchanges to help small businesses and uninsured individuals gain affordable coverage — take effect in 2014.
McPherson and Morrone say Maine employers increasingly want to know when this year's ACA deadlines are and what they must do to meet them. That's especially true, they say, for the small- and mid-size employers that comprise roughly 97% of the businesses in the state. Here's a primer:
1. Determine if you are a small or large employer
When to do it: Now.
Caveat: It's not as simple as you think.
Step 1, McPherson says, is for companies to do the math and determine exactly how many employees they have, since the answer to that question will guide all the other steps. The essential question employers need to answer is whether their company is “small” vs. “large” as defined by the ACA law:
- Small employers have fewer than 50 full-time employees (determined by counting the number of employees in the prior year). They face no penalty for not offering health insurance coverage, and employees will not be eligible for incentives such as a tax credit or subsidy when their employer makes a contribution toward group health insurance.
- Large employers have 50 or more full-time employees (or 50 full-time equivalent employees) and can be penalized if their full-time employees are not offered what the ACA law describes as “minimum essential coverage” — meaning, the plan must pay at least 60% of the expected health care costs, with the remaining 40% paid by the employee through co-pays, deductibles or co-insurance.
But McPherson and Morrone quickly acknowledge that determining whether a company has 50 or more full-time employees is anything but simple. Here's how to calculate the number of employees:
- “Full time” is defined as working an average of 30 hours per week. So if a company has 40 employees working a traditional 40-hour week, but has 10 more employees working at least 30 hours per week, under the ACA's definition it has 50 “full time” employees and qualifies as a “large” employer.
- McPherson and Morrone say employers also must calculate how many full-time equivalent, or FTE, employees they have. There are two steps involved: 1.) Calculate the aggregate number of hours of service in a month for each part-time employee (“part-time” meaning no more than 120 hours of service per month). 2.) Divide those total hours of service by 120. That's the number of FTEs for that month. For example, for a company with 40 full-time employees that also has 15 part-time employees, each working 25 hours per week, the calculation goes like this: Total hours of service for 15 part-time workers equals 1,500 aggregate hours (25 hours per worker multiplied by four weeks = 100 hours a month per worker multiplied by 15). Divide 1,500 by 120 and it equals 12.5 FTEs. Add that number to 40 full-time workers and the company qualifies as large with 52.5 FTEs employed.
“We have certainly run into a number of groups that initially thought they were a small business, only to find out that they aren't,” says McPherson.
She adds that seasonal employees don't need to be counted if the employer only exceeds 50 full-time employees for 120 or fewer days during the calendar year, and the only reason the employer exceeds 50 employees is because of the seasonal employees.
A regulation released in December 2012, she says, allows employers to look back six consecutive months in 2013 to calculate their large or small status for 2014, when large employers will be mandated to provide health coverage for their full-time employees or else risk a penalty.
Portland lawyer Emily Cooke, a member of the health care services team at Portland law firm Pierce Atwood, says business owners who think they're on the fence should exercise “a lot of caution” before deciding they're small and therefore not subject to the ACA's large employer requirements. There are additional nuances to the large-or-small question, such as the impact of seasonal workers, that must be analyzed before an employer can truly say he's off the hook of the ACA's pay-or-play requirement, the stick to the federal government's carrot that imposes penalties if large companies don't offer coverage.
“At this point there's not a set definition for seasonal employee,” says Joanne Pearson, a Portland lawyer who also serves on Pierce Atwood's health care services team. “You are required to make a good-faith determination of what 'seasonal' means [for your business] … The rules are complex. If you're not sure, it's best to red flag anything you might be tripping on and seek guidance on those issues.”
Cooke, for example, says employers owning two or more companies should check Internal Revenue Service regulations to see if they are part of a controlled group. The ACA specifies that employees of controlled groups are to be lumped together, with separate companies being treated as a single employer. The combined employee numbers could put the employer in the large employer group and therefore subject to the ACA's pay-or-play requirements.
“The IRS has signaled that it will be expansively interpreting the term 'employee' and there will likely be unfavorable anti-abuse rules in the final regulations,” cautions Pearson. “Employers that believe they are not covered by the rules should pay close attention to the proposed and final regulations in order to avoid any unpleasant surprises down the road.”
2. Do you play or pay?
When to decide: Now.
Caveat: Health care benefits remain a huge recruiting tool, so changes based on ACA mandates are unlikely.
Once the large-or-small question is answered, an employer having 50 or more full-time employees can still choose to pay a fine rather than offer coverage to 95% of its full-time employees (play).
“It's a business's choice,” and the ACA takes that into account, says Cooke.
Not surprisingly, there's math involved in determining how much of a penalty the large employer will have to pay for not offering health insurance to its full-time employees (there's no requirement to offer it to part-time workers).
Step 1 involves the employer choosing whether to offer or continue health coverage to full-time employees. The ACA sets two conditions: 1.) Is it affordable (its cost cannot exceed 9.5% of an employee's wages)? 2.) Does it offer the minimum essential services? (i.e., the employer covers at least 60% of the cost of benefits)?
If health coverage is offered but one or more full-time employees can't afford it and those employees qualify for a tax credit or premium subsidy through a public health exchange, the employer must pay a $3,000 annual penalty for each FTE not covered by the company policy.
Large employers who don't offer any health coverage will face a $2,000 annual penalty for each employee beyond the first 30 uncovered employees. For example, a company with 50 FTEs choosing not to offer health coverage would face a $40,000 penalty. Here's the math: 50 minus 30 equals 20; 20 multiplied by $2,000 equals $40,000.
Cooke and Pearson believe few, if any, Maine companies exceeding the 50 FTE threshold and already offering health coverage will be tempted to lay off workers or cut those benefits to avoid the ACA's pay-or-play requirements. That's also true, they say, for mid-size companies already providing health insurance.
“They want to be competitive,” Pearson says of both groups, explaining that good health care benefits are an essential way of hiring and keeping top-flight employees.
3. What’s up with Maine’s health care exchange?
When: Enrollment starts Oct. 1; coverage effective Jan. 1.
Caveat: Details of the small business plan remain in flux; tax incentives expire in three years.
Ellen McPherson says Employee Benefits Solutions has been encouraging its clients to pay particular attention to communicating with their workers as companies move toward their policy renewal dates. For smaller companies that either don't offer health insurance or are planning to utilize Maine's Health Insurance Exchange that will open for business on Jan. 1, 2014, the ACA requires employers to notify employees that the exchange's open enrollment period will begin Oct. 1.
Besides providing a marketplace for uninsured people to make side-by-side comparisons of different health plans, the state's Health Insurance Exchange will operate a Small Business Health Options Program, or SHOP, focusing on the needs of small businesses.
Cooke says the SHOP exchange is intended to increase the options for small businesses wanting to provide health insurance for their employees. Putting small businesses into the same insurance pools, in theory, gives them more purchasing clout and is expected to lower insurers' administrative costs by spreading the burden across more employers. The ACA also requires all SHOP plans to provide detailed information about prices, benefits and the level of coverage provided, making apples-to-apples comparisons easier for the small employers and their workers.
The exchange will start with one plan when it opens Jan. 1, 2014, and develop more options in 2015. Through the end of this year, the federal government is offering a small business premium tax credit of up to 35% of the company's share of the employees' premium costs. To be eligible, a company must:
- Have fewer than the equivalent of 25 full-time workers.
- Have an annual average employee wage below $50,000.
- Cover at least 50% of the cost of health insurance.
Starting in 2014, the maximum tax credit increases to 50% of the employer's share of health insurance coverage, but will be available only to small businesses purchasing coverage through SHOP. That tax credit will be available for two years.
The non-partisan Congressional Budget Office estimates that approximately 2.6 million small business employees will get coverage through the exchanges in 2014, increasing to approximately 3.7 million employees in 2017 (in part because SHOP eligibility will expand nationwide to all businesses with 100 or fewer FTEs instead of the current provision allowing states to limit participation to businesses with up to 50 employees).
With so many variables and unknowns, Employee Benefits' Morrone says it's too early to predict whether the ACA will achieve its goal of lowering health insurance costs while expanding coverage to almost 50 million uninsured Americans.
Employers currently offering health benefits might find that segment of their work force will grow due to the ACA's definition of a full-time employee, he says. Likewise, those employers will have to make sure their contribution strategy for premium costs continues to meet the ACA's affordability standard. Some employers, he says, will be looking closely to see if they can continue meeting that if the number of their full-time employees dramatically increases.
Cost is only one way to look at the ACA's impact on their business, Morrone says. The other is to look at what's needed to run the business. For many companies, that means offering health coverage to retain the skilled workers they need to be competitive.
Either way, this is the year businesses will be making important decisions about how they'll be meeting the ACA's requirements. “You can't wait any longer,” Morrone says.











Comments