
Recruiting — and retaining — physicians gets more strategic amid shrinking workforce
Later this month, Jessica Kwock will start as a dermatologist with InterMed PA, Maine's largest physician-owned primary-care practice that employs close to 100 doctors in Portland, South Portland and Yarmouth.
Kwock, 36, who grew up near Boston, recently moved to Maine from Charlottesville, Va., after a fellowship at the University of Virginia Medical Center. She and her husband, an anesthesiologist, both searched for jobs in northern New England to be closer to family, with Portland high on their list.
“It had everything we were looking for,” says Kwock, who will be based at Intermed's South Portland branch where she looks forward to working with general practitioners and to applying her clinical skills.
“They seemed very supportive of enabling me to practice medicine in a way that I felt would best benefit my patients and also provide professional satisfaction,” she says, “whereas perhaps in a smaller practice I wouldn't necessarily have been able to do that.” She interviewed for the job in November and accepted in March, while her husband was hired by Spectrum Medical Group in Portland.
With demand for doctors outpacing supply nationwide, and the crunch particularly acute in Maine, many employers are recruiting more strategically, launching searches well ahead of anticipated openings, using staff doctors to reach out to potential job candidates, and focusing on workplace culture. They're also picky about who they hire.
“There have been physicians that we've recruited over the years who in all likelihood would have made a lot of money for the practice who were not a fit, and there's no question we made the right decision in not extending them a contract,” says InterMed CEO Dan McCormack. He expects to ramp up hiring in coming months as he scouts greater Portland for a fourth location. “We need more space.”
A shrinking pool of candidates
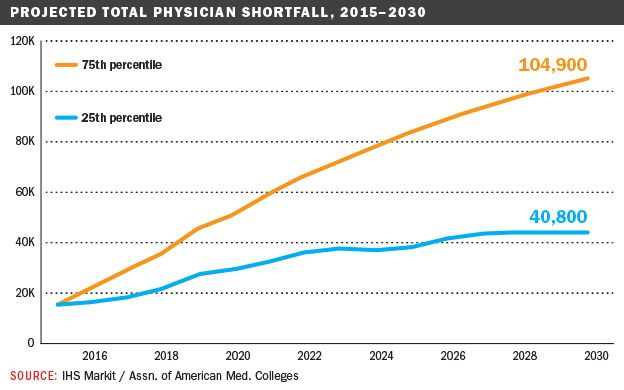
The pool of attractive candidates will only get smaller amid a looming nationwide doctor shortage, driven by an aging population and an aging physician workforce. Between 2015 and 2030, the Association of American Medical Colleges projects a shortage of between 40,800 and 104,900 doctors. The lower estimate is only realistic if there are aggressive changes to care delivery patterns and widespread delayed retirement by today's doctors.

The group projects a shortage of between 7,300 and 43,100 primary care doctors, making it difficult for millions of people to get preventive health care services, and an “equally troubling” shortage of between 33,500 and 61,800 specialists, affecting growing numbers of older patients with Alzheimer's disease, cancer and heart conditions.
Maine, already the oldest state with a median age of 44.5 (nearly seven years above the U.S. figure) and nearly a third of its active physicians age 60 and older, not to mention a large rural population, looks to be hit especially hard. The Maine Department of Labor estimates that about 9,000 more jobs will be needed in healthcare and social assistance by 2024, already the largest employer with a total of 100,000 employees in 2014.
While there are various myths surrounding the expected shortfall, Jonathan Harvey, a doctor who serves as chief medical officer at Martin's Point Health Care, doesn't think the numbers are off.
“We don't think the predictions are exaggerated at all in light of the aging population that we serve in Maine,” he says. “Folks need more medical care as they get older, and at the same time you have a trend where physicians and nurse practitioners are wanting to work parttime. These factors lead to a relative scarcity of primary care providers, and physicians in general, and causes organizations to think strategically about how they recruit and more specifically about how they deliver the needed care more efficiently.”
At Martin's Point, a nonprofit that employs close to 40 physicians across six locations in Maine — three of which were opened in the past five years — and one in Portsmouth, N.H., that strategic thinking includes recruiting doctors who can effectively work on teams with other medical staff and proactive recruiting.
“It used to be we would wait for an opening before placing an ad or posting a position,” Harvey says. “Now we're looking to hire folks well in advance of their start date. It's not unusual to engage high potential candidates two years ahead and to then hire a full year in advance.”
He adds that having an in-house recruiter makes it possible “to authenticate the message about our culture” and “allows us to plan a more strategic approach and to adjust more quickly to business needs.”
MaineHealth's power recruiters
MaineHealth does the same on much grander scale for the entire state, with a team of recruiters working on talent acquisition for member hospitals from its flagship Maine Medical Center in Portland to Pen Bay Medical Center in Rockport and Waldo County General Hospital in Belfast.
Besides offering specialized or tertiary care, Maine Med is also a teaching hospital, offering residencies in anesthesiology to urology and fellowships in areas such as cardiology, geriatrics, infectious disease and sports medicine.
As director of the MaineHealth Physician Recruitment Center, Alison C. Nathanson oversees talent acquisition at all member hospitals, working closely with recruiters at each institution with whom she meets quarterly. She joined MaineHealth in 2010 after more than three years at Southern Maine Health Care and more than a decade in New York City as director of recruiting for the law firm Covington & Burling.
Nathanson finds medical recruiting to be much more rewarding “because you're bringing someone into the state who is going to help people who live here, and they're going to provide care.”
Susan Pelletier, vice president of human resources-shared services for all 18,000 MaineHealth employees, says the centralized recruiting works well. “Rather than stand-alone hospitals dealing with their own challenges, under Alison's leadership we've really come together so that we can make the most of every candidate in helping them find the setting that is best for them and meets their needs. That really has been a more powerful approach, because the shortages are different in our different communities.”
At the same time, MaineHealth faces the same recruiting challenges as its peers, so it also plans for openings at least a year in advance and keeps a central database of 1,500 resumes, with notes on whether there's an interest in Portland or a rural hospital. “It's constant and it's fun,” says Nathanson, “because some people will come back around again two or three years later and say, 'I talked to you a couple of years ago and now I'm ready to look,' or 'Our plans have changed and we are coming to Maine.' That's nice, too.”
MaineHealth recruiters also go to national career fairs (including one at Maine Med) to promote both MaineHealth and Maine's quality of life, handing out brochures like one showing an osteopath fly-fishing against a big open sky. But they've found that physicians themselves make the best recruiters, whether at conferences or informally reaching out to peers. “Physicians want to talk to physicians,” notes Pelletier. The efforts have led to 40 new doctor hires over the past year, “which on a base of 900 and change is significant.” Nathanson adds that “it's more growing, not replacing.”
Addressing rural needs
Maine Med isn't just a teaching hospital for future MaineHealth positions. In partnership with Tufts University School of Medicine, it set up a program called Maine Track in 2008 to address the state's doctor shortage, particularly in primary care and in underserved rural communities. Maine residents and those with ties to the state and rural practice are given preference, and financial aid is available. A second program, launched in July with one resident and known as the Rural Internal Medicine Track, blends experiences of training at Maine Med in Portland and Stephens Memorial Hospital in Norway, part of MaineHealth.
Out of the 32 people in the first Maine Track graduating class of 2013, 64% are now practicing in Maine. Among them is 31-year-old Little Cranberry Island native Marya Goettsche Spurling, who always wanted to be a doctor and practice in a small town, so Maine Track was perfect. “I absolutely would recommend it,” she says. “Focusing on students who come from places in rural Maine is really crucial, since we're the ones who are most likely to return.” She now practices family medicine at Redington-Fairview General Hospital in Skowhegan, where her variety of responsibilities includes delivering babies, “a valuable part of my job I really enjoy.”
Meanwhile at Mayo Regional Hospital in Dover-Foxcroft, president and CEO Marie Vienneau says she just hired an internist who went through Maine Track and bought a house close to his wife's grandparents. “It's very encouraging to see that happen,” she says. Nevertheless it can be difficult filling posts especially in the emergency department, where she often relies on doctors doing temporary stints of up to three months, at three times the cost of an employee. “If you're talking about the rural workforce,” she says, “it's not only physicians that are challenging, but also nurses and physical therapists.”
The University of New England College of Osteopathic Medicine also offers training in primary care and rural medicine, and has more alumni practicing in health-profession shortage areas in Maine than Tufts, the University of Vermont and Dartmouth College combined, according to its dean, Jane Carreiro. She insists that the school does not compete with Maine Med or Tufts or even Boston. “The health profession needs people in city centers as well as those practicing in rural areas,” she says. “In the end, we're all just trying to recruit the best possible people to take care of their neighbors, the people of Maine.”
















Comments