Soaring health care costs drive consolidation of Maine's hospitals
Escalating costs have driven consolidation of hospitals and other health care facilities into sprawling systems over the past 25 years.
At the same time, new standards in services and new technologies are driving significant growth at urban facilities like Maine Medical Center. That’s happened even while many rural facilities have cut back on services in response to declines in patients and revenue.
In the 1990s, Maine didn’t have systems like MaineHealth, Northern Light and Central Maine Healthcare.
“The affiliation of smaller hospitals with larger hospitals has been a monumental change,” says Steven Michaud, president of the Maine Hospital Association.
The topic of cost-containment in health care is not new. But by the 1990s, it was driving hospital collaboration and consolidation. By the late 1990s, hospital and health care systems began to form in earnest, changing the way care is delivered, according to the Maine Hospital Association.
The 2003 Dirigo Health Reform Act aimed to reduce the growth of health care costs and increasing quality and access. Expansion of the state’s Medicaid program ensued.
Health care employment has grown every year since 1992, even in economic downtimes, including the most recent recession. Maine’s demographics — its aging population — will keep the health care workforce growing.
One issue is that Maine’s health care workforce also aging. As nurses and other practitioners retire, there are not enough trained workers to fill the jobs.
Hospitals band together
Consolidation of hospitals and hospital groups has been the primary strategy to contain costs and mitigate workforce shortages, Michaud says.
Today, 60% of Maine hospitals are part of systems. The number is growing. Two factors are escalating costs and cuts in insurance payments.
“That led them to start banding together,” he says. “A lot of it, also, is the drive to better coordinate safer and more efficient care.”
Brewer-based Eastern Maine Healthcare System’s 2018 rebranding as Northern Light Health was a reflection of that evolution, from individual locations to integrated health delivery with coordinated statewide offerings. Northern Light’s growing network of hospitals comprises nine member hospitals and more than 100 health care and home care sites.
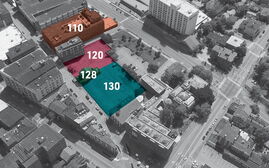
MaineHealth similarly evolved its network in response to challenges facing local health care delivery sustainability. New England’s largest integrated health system, founded in 1998, MaineHealth is also Maine’s largest private employer. It became a single, seven-hospital nonprofit system this year. Momentum for further growth remains strong, with Mid Coast-Parkview Health in Brunswick considering joining the system and Maine Med’s $500 million modernization and expansion moving forward.
In 2013, MaineGeneral underwent similar modernization when it opened its $312 million Alfond Center for Health in Augusta. And Mercy Hospital in Portland is moving closer to consolidating operations and services on an expanded Fore River campus.
In rural Maine, though, provider numbers have declined. Two big factors have helped preserve rural hospitals, says Michaud. One is affiliation with the systems. Another was the federal government’s creation in 1997 of the Critical Access Hospital program, which allows designated hospitals to receive benefits such as cost-based reimbursement for Medicare services, thus reducing their financial vulnerability and improving access to health care.
“If that program had not happened, we’d have far fewer hospitals in rural Maine,” says Michaud.
But new challenges, like declines in population and hospital use, affect rural hospitals. Michaud expects trends to will continue.
“The state and federal governments continue to be strapped for money,” he says. “That continues to put extraordinary pressure on Medicare and Medicaid — our biggest payers. We look to the future and see there’s no new money coming in anywhere. It causes us to continue to find ways to do things more efficiently and cut costs where we can.”














0 Comments